In the evolving field of orthopedic medicine, bunion management stands at the intersection of biomechanics and modern medical technology. A bunion, formally termed hallux valgus, is a painful bony protrusion that forms at the base of the big toe. With the rise in cases attributed to genetics, improper footwear, and systemic conditions like arthritis, the demand for high-precision bunion medical devices has never been greater.
Modern solutions for bunions no longer rely solely on invasive surgical corrections. Thanks to advancements in materials science, biomechanical engineering, and orthopedic innovation, today’s devices offer targeted support, pain relief, and often, long-term structural realignment.
Understanding the Bunion Condition
A bunion develops when the first metatarsal bone drifts outward while the big toe moves inward toward the other toes. This misalignment causes the joint at the toe’s base to swell and become painful. Over time, cartilage erosion, joint stiffness, and increased friction from footwear can severely impair function.
Bunions are not merely cosmetic concerns but progressive structural deformities caused by biomechanical imbalance. As such, addressing them requires precision tools that relieve symptoms and restore proper gait dynamics.
The Role of Medical Technology in Bunion Management
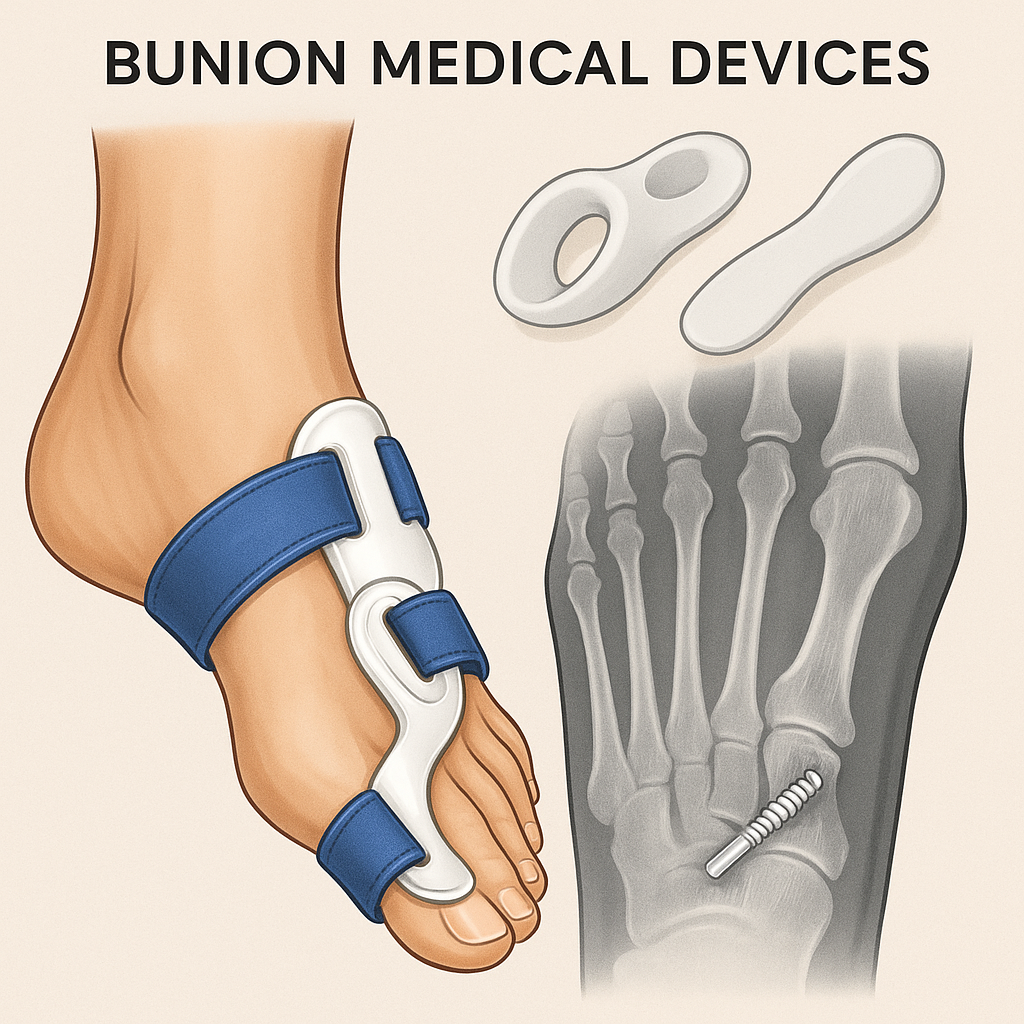
Medical technology has drastically enhanced our ability to treat bunions without relying exclusively on open surgical procedures. Innovative bunion medical devices now include:
Orthotic devices for biomechanical realignment
Minimally invasive fixation systems for surgical correction
Smart wearable solutions for dynamic monitoring and therapy
Pressure-distributing insoles to prevent progression
These advancements prioritize practical use, everyday comfort, and personalized care for the patient.
Non-Surgical Bunion Devices: Science-Driven Solutions
Dynamic Splints and Night Correctors
Technologically enhanced splints are fabricated using memory foam, thermoplastics, and breathable fabrics that adapt to individual foot anatomy. These are worn overnight or during rest periods to realign the metatarsophalangeal joint slowly.
Modern dynamic splints offer:
Customizable tension straps are designed to gradually correct toe misalignment.
Articulated joints maintain mobility.
Skin-friendly linings that minimize irritation during prolonged use
Some newer models even integrate microelectronic sensors that assess toe alignment progress over time.
Silicone Toe Separators with Medical-Grade Materials
Silicone separators were once simple buffers between toes. Now, through material science, they’ve evolved to include:
Antimicrobial, medical-grade gels
Anatomical shaping based on 3D foot scans
Biocompatible coatings to prevent allergic responses
They play a vital role in alleviating pressure, enhancing blood flow, and supporting the healing of soft tissues.
Orthopedic Insoles and Custom Footbeds
Using gait analysis and pressure-mapping systems, medical labs can design insoles tailored to redistribute weight away from the bunion site. These insoles feature:
Multi-layered polymers for shock absorption
Embedded arch supports correct overpronation.
Zoned pressure pads to offload the first metatarsal head
These devices slow bunion progression and are often paired with physical therapy.
Surgical Innovations: High-Precision Bunion Correction
For advanced bunion cases, surgical technology has seen significant refinement. Innovations now offer options that reduce recovery time, minimize scarring, and maintain foot integrity.
Minimally Invasive Bunion Surgery (MIBS)
MIBS uses tiny incisions and fluoroscopic guidance to correct bone alignment. Specialized burrs and fixation devices allow for precise bone cuts without major tissue disruption.
Benefits include:
Lower risk of infection
Faster return to weight-bearing activities
Smaller surgical scars
2. Internal Fixation Devices
Advanced bunion medical devices such as memory compression screws and low-profile plates are used for osteotomy fixation. These are made from titanium alloys or bioresorbable polymers.
Their biomechanical design ensures:
Optimal bone healing
Stable correction angles
Reduced need for revision surgeries
These surgical aids are the backbone of modern bunion procedures, helping orthopedic surgeons achieve durable results.
Post-Operative Devices and Smart Recovery Aids
Healing doesn’t end in the operating room. Technology has improved post-operative care through:
Smart footwear that monitors plantar pressure distribution
Rehabilitation boots with adjustable dorsiflexion angles
Biofeedback-enabled insoles for gait retraining
These tools empower patients to engage in active recovery while minimizing reinjury risks.
Research and Data Integration in Device Design
With AI and machine learning integration, researchers can now study thousands of bunion cases to refine device prototypes. Data from pressure mats, wearable sensors, and digital foot models are fed into predictive algorithms, helping engineers create:
Gender-specific designs
Devices suited to various arch types
Regionally customized solutions based on climate and footwear norms
Regulatory Compliance and Safety Standards
Every bunion medical device must comply with strict international regulations, such as:
FDA Class I & II classification for orthotic devices
CE marking for European distribution
ISO 13485 certification for quality management systems
These standards ensure devices are effective and safe for long-term use.
Practical Considerations When Choosing a Bunion Device
When selecting a device, both patients and clinicians should consider:
Severity of deformity: Mild cases may respond well to toe spacers and splints; severe cases may need surgical intervention.
Activity level: Athletes may benefit from dynamic orthoses that allow movement while offering correction.
Material allergies: Always choose devices made from hypoallergenic, biocompatible materials.
Cost vs. durability: Medical-grade devices may have higher upfront costs but offer superior outcomes.
The Interdisciplinary Approach to Bunion Care
Today, bunion treatment involves:
Orthopedic surgeons for diagnosis and surgical planning
Podiatrists for conservative care and gait analysis
Physical therapists for recovery and strengthening
Biomedical engineers for device innovation
This holistic model ensures each stage of care is optimized through technology.
Looking Forward: The Future of Bunion Technology
With emerging technologies like 3D-printed implants, nanomaterial insoles, and IoT-connected wearables, the future of bunion medical devices is incredibly promising. These innovations aim to:
Enable fully personalized treatment plans
Reduce the need for surgical intervention.
Enhance patient comfort and compliance.
Furthermore, crossover research in hernia mesh design and orthopedic biomechanics has influenced bunion device development. To see how similar technology is being applied in other medical domains, explore this insightful article:
👉 Inguinal Hernia Medical Devices: Advances in Mesh and Repair Tech
Conclusion
Rapid advancements in medical technology have transformed the landscape of bunion medical devices. From non-invasive orthotic solutions to state-of-the-art surgical instruments, patients today have access to a wide range of tools that relieve pain and restore alignment and mobility.
As medical research drives innovation, the future holds exciting possibilities for even more personalized and effective bunion care. With the right device and a tech-enabled treatment plan, lasting relief is well within reach.