In today’s technologically advanced era of cardiovascular medicine, precision diagnostics and non-invasive tools have transformed how arrhythmias are understood and managed. Among the many conditions detected through modern techniques, one of the more subtle but clinically significant findings is the wandering pacemaker.
Though often benign, this shifting pacemaker activity offers deep insight into atrial function and conduction behaviour. This article explores the phenomenon from a diagnostic technology standpoint, focusing on how state-of-the-art tools support early detection, interpretation, and risk stratification.
What is a Wandering Pacemaker?
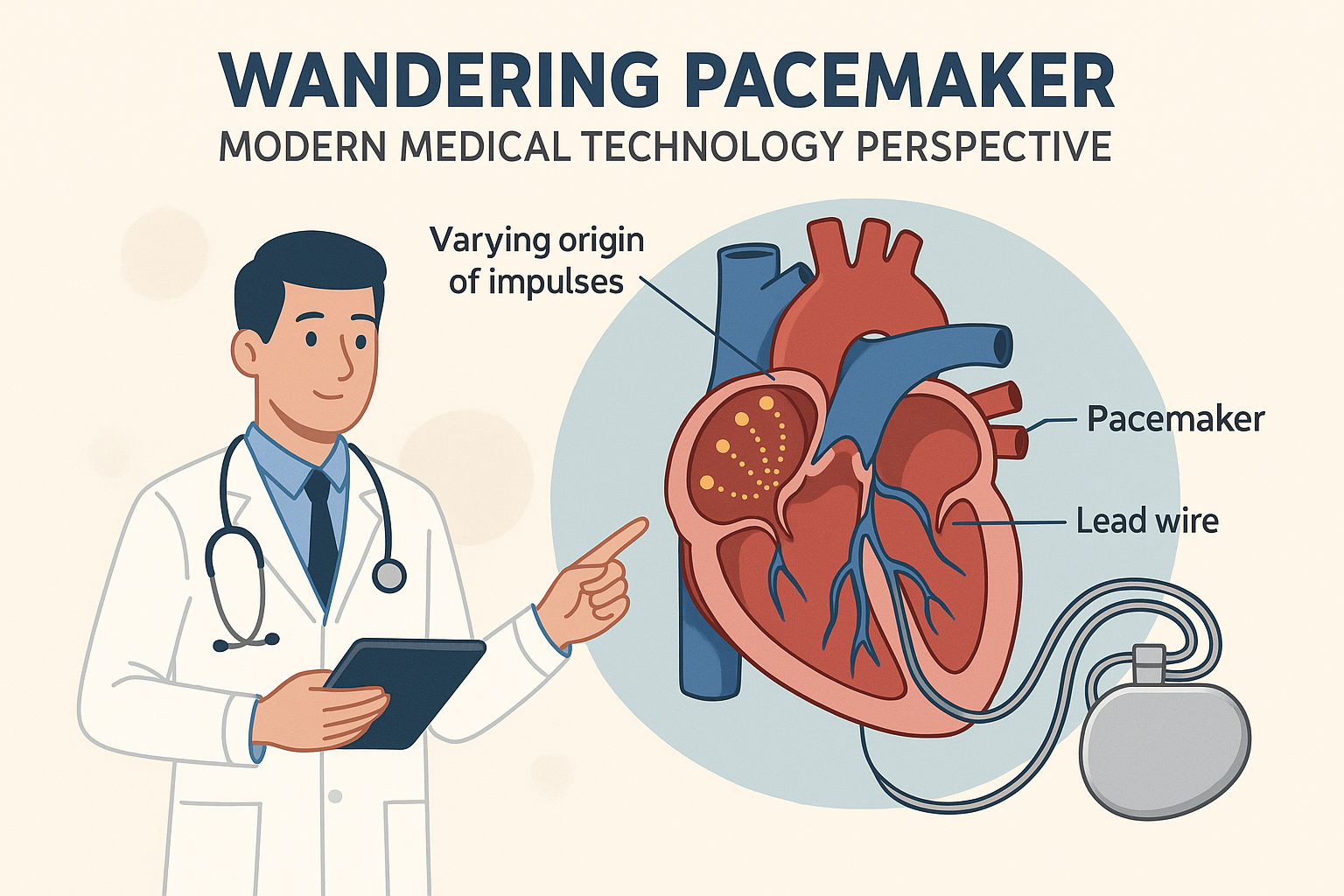
A wandering pacemaker, medically referred to as a wandering atrial pacemaker (WAP), is a type of atrial arrhythmia where the natural pacemaker of the heart, the sinoatrial (SA) node, shifts its control temporarily to other ectopic sites in the atria. This results in fluctuating P-wave morphologies on an electrocardiogram (ECG), typically indicating the changing origin of electrical impulses within the heart.
With the heart rate generally under 100 beats per minute, WAP is often asymptomatic and discovered incidentally, especially during routine ECGs or advanced rhythm monitoring using wearable or ambulatory technology.
The Role of Modern Diagnostic Tools
In the past, detecting a wandering pacemaker relied heavily on a standard ECG performed in clinical settings. Today, medical technology has revolutionised the way these arrhythmias are observed and monitored:
High-Resolution Digital ECGS
Modern ECG machines provide high-resolution tracings capable of identifying the subtle differences in P-wave shapes that define WAP. These devices often include artificial intelligence (AI)-driven algorithms that alert clinicians to variable atrial activity, prompting further evaluation.
Ambulatory ECG Monitoring
Portable devices like Holter monitors and patch-based systems can record heart rhythms over extended periods. These are particularly effective in detecting transient WAP episodes that may not be present during a standard 10-second ECG.
AI and Machine Learning Integration
With the integration of AI, rhythm irregularities such as wandering pacemakers can be detected automatically. Machine learning models trained on large datasets can distinguish between WAP and similar arrhythmias, improving diagnostic accuracy.
Electrophysiological Features on ECG
The core diagnostic tool remains the electrocardiogram, with a wandering pacemaker identified by:
Three or more distinct P-wave morphologies in a single lead.
Variable PR intervals, due to differing distances from atrial pacemaker sites to the AV node
Normal QRS complexes, indicating the ventricles are unaffected
A heart rate below 100 bpm, distinguishing WAP from multifocal atrial tachycardia (MAT).
Advanced software now allows automatic detection and flagging of P-wave variations, reducing the risk of misinterpretation.
Why It Matters: Clinical and Technological Insights
While WAP is usually benign, its detection holds clinical and technological significance:
Indicator of Atrial Health
WAP may indicate underlying atrial irritability. This is especially relevant in patients with chronic respiratory conditions, electrolyte imbalances, or early signs of structural heart disease.
Monitoring the Elderly and Athletes
In elderly patients, WAP may reflect degenerative conduction system changes. In athletes, enhanced vagal tone can trigger WAP during rest. Continuous monitoring helps differentiate normal physiology from pathology.
Drug and Device Monitoring
Drugs like digoxin or beta-blockers can influence atrial rhythm. Healthcare providers now employ implantable loop recorders and remote cardiac telemetry systems to ensure medications do not unintentionally induce arrhythmias like WAP.
Medical Technology in Risk Stratification
Thanks to evolving diagnostic protocols, patients with wandering pacemakers can now be assessed more precisely for potential progression to:
Multifocal atrial tachycardia
Atrial fibrillation
Bradyarrhythmias requiring pacing
Imaging and Diagnostic Correlation
In cases where WAP raises concern for atrial dilation or structural heart changes, cardiac imaging is used in conjunction with ECG findings:
Echocardiography evaluates atrial size and function.
Cardiac MRI gives high-resolution insight into atrial tissue health, fibrosis, and conduction pathways.
For non-cardiac influences, particularly in patients with overlapping symptoms, tools like MRI defecography can help assess pelvic-floor disorders that indirectly affect cardiovascular function via autonomic imbalance.
To learn how MRI defecography supports medical diagnostics beyond cardiology, see our guide on MRI Defecography: Harnessing Medical Technology to Diagnose Pelvic Floor Disorders.
Wandering Pacemaker vs. Other Arrhythmias
Understanding WAP also requires distinguishing it from similar atrial arrhythmias:
| Feature | Wandering Pacemaker | Multifocal Atrial Tachycardia |
| Heart Rate | <100 bpm | >100 bpm |
| P-wave Morphologies | ≥3 in a single lead | ≥3 in a single lead |
| Regularity | Irregular | Irregular |
| Clinical Context | Often healthy individuals | Common in COPD, the elderly |
| Management | Often none | May require rate control or therapy |
Advanced arrhythmia classifiers embedded in ECG software can automatically make such comparisons and flag anomalies for cardiologist review.
Management Strategy
Most cases of wandering pacemakers do not require direct intervention. Instead, modern clinical protocols supported by medical technology emphasise:
Observation and Lifestyle Monitoring
Using smart wearable devices, patients can be monitored for rhythm variability, helping providers track frequency and significance without hospital visits.
Correction of Underlying Causes
Identifying and correcting potential triggers such as:
Electrolyte disturbances
Medication side effects
Sleep apnea
Dehydration or stress
Risk-Based Follow-Up
Advanced patient management platforms can set alerts for:
Escalating heart rate trends
Onset of new arrhythmias
Decreasing heart rate variability
This ensures that the wandering pacemaker remains benign and does not evolve into a more serious condition.
A Technological Case Study
Consider a 62-year-old patient with mild COPD and occasional palpitations. A modern clinic might deploy:
A high-resolution digital ECG detects three varying P-waves
A 48-hour Holter monitor confirming intermittent WAP episodes
An AI-generated ECG report suggesting a low-risk profile
Cardiac imaging (e.g., MRI or echo) confirming normal atrial structure
The final diagnosis: benign WAP with no immediate intervention needed, demonstrating how layered medical technology provides clarity and peace of mind.
Future Outlook: Digital Health and Cardiac Electrophysiology
With the integration of remote monitoring, telehealth, and machine learning, the future of arrhythmia management is shifting toward early detection and patient empowerment. Wandering pacemaker is just one example of how subtle rhythm variations can be uncovered, contextualised, and monitored continuously, all thanks to breakthroughs in medical diagnostics.
As algorithms become more refined and device integration becomes more seamless, even incidental findings like WAP will play a bigger role in shaping comprehensive cardiovascular care.
Conclusion
The wandering pacemaker may seem minor in the grand scope of cardiology, but with modern medical technology, its discovery and interpretation have become both easier and more clinically relevant.
From AI-driven ECGS to wearable rhythm trackers and imaging-assisted analysis, the tools at our disposal today ensure that even benign arrhythmias are not overlooked. This not only supports better heart health but also integrates seamlessly with broader health systems focused on prevention, personalisation, and proactive care.
For those exploring the intersection of cardiology and diagnostic imaging, don’t miss our related discussion on MRI Defecography: Harnessing Medical Technology to Diagnose Pelvic Floor Disorders, a prime example of how diverse medical technologies converge for holistic patient care.