Inguinal Hernia Medical devices: Inguinal hernias rank among the most prevalent types of abdominal wall hernias, impacting millions of people around the globe. With increasing innovations in medical technology, the approach to diagnosing and treating inguinal hernias has evolved dramatically, particularly in medical devices used for surgical repair.
This article explores the inguinal hernia condition, the evolution of hernia repair using medical devices, and how technologies such as surgical mesh are revolutionizing patient outcomes. We’ll also examine the safety, effectiveness, and controversies surrounding these devices to provide a full understanding of the current landscape.
What Is an Inguinal Hernia?
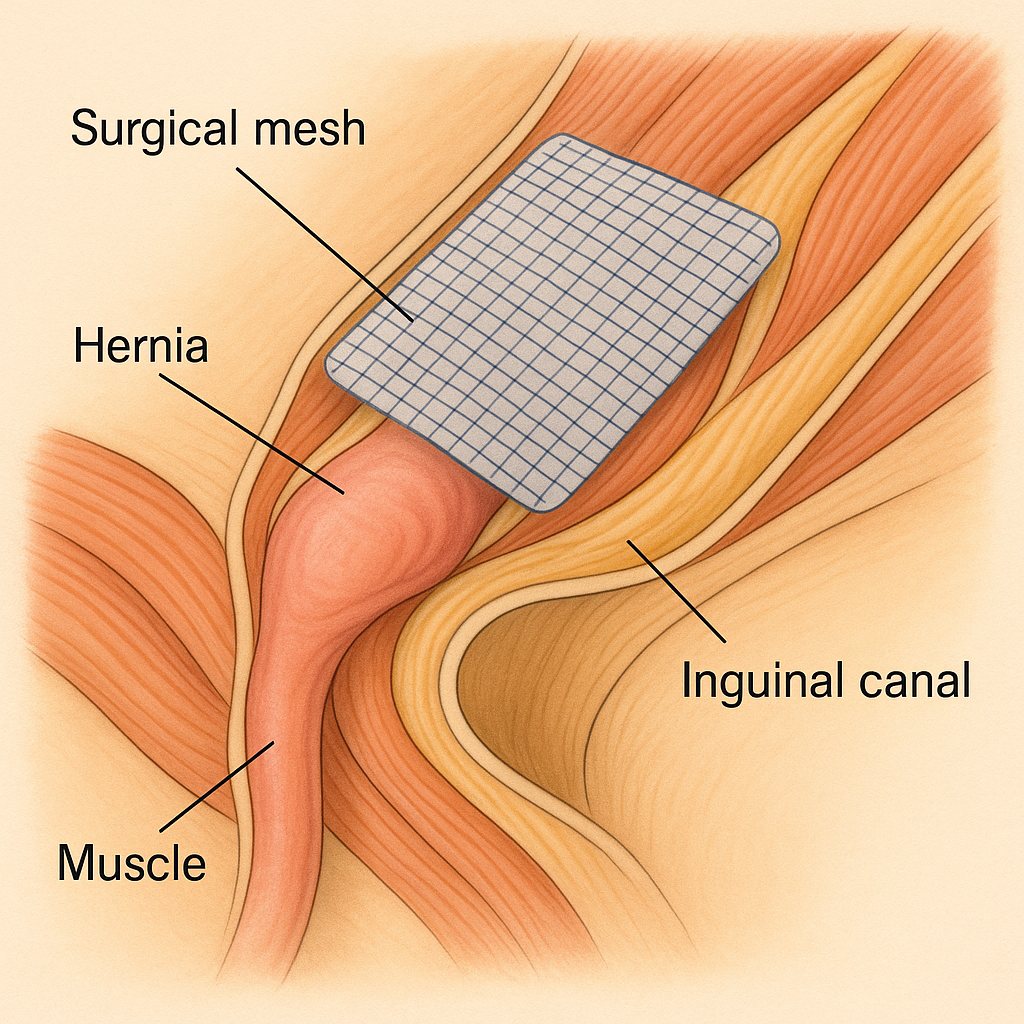
An inguinal hernia occurs when soft tissue, usually part of the intestine, protrudes through a weak spot or tear in the lower abdominal wall, often into the inguinal canal. This condition is more common in men due to natural anatomical differences. Symptoms may include:
A visible bulge in the groin
Pain or discomfort during activities such as lifting, coughing, or bending.
Weakness or pressure in the groin area
While not always dangerous, untreated hernias can lead to complications such as incarceration or strangulation, making surgical intervention essential.
Evolution of Medical Technology in Hernia Repair
Hernia repairs have been performed for over a century, but medical advancements have dramatically improved their safety and success. A major advancement in this field has been the introduction of surgical mesh.
Traditional Repair vs. Mesh Repair
Traditional Repair (Herniorrhaphy): Involves suturing the muscle tissue together without implants.
Mesh Repair (Hernioplasty): Involves placing a synthetic or biologic mesh over the weakened area to reinforce it.
Studies show that mesh repair significantly reduces the risk of recurrence and shortens recovery time, making it the gold standard in modern hernia repair.
Surgical Mesh: The Cornerstone of Inguinal Hernia Medical Devices
Surgical mesh is a medical-grade implant, usually made from polypropylene or absorbable polymers. It is designed to provide support and allow tissue integration for long-term strength.
Types of Mesh Used:
Synthetic Non-Absorbable Mesh: Permanent support (e.g., polypropylene)
Synthetic Absorbable Mesh: Breaks down over time (e.g., polyglycolic acid)
Biologic Mesh: Derived from animal or human tissue, used in contaminated fields
How Mesh Works in Inguinal Hernia Surgery
Mesh is inserted through either an open surgery or a laparoscopic procedure, depending on the patient’s needs. Once implanted, it acts as a scaffold, allowing natural tissue to grow into it, strengthening the abdominal wall and reducing the chance of recurrence.
Benefits of Mesh Technology:
Lower recurrence rates
Shorter hospital stay
Less postoperative pain
Faster return to normal activities
FDA Insights: Regulation and Safety
The U.S. Food and Drug Administration (FDA) closely monitors the development and performance of surgical meshes. According to their database, most meshes in hernia repair have undergone stringent testing for biocompatibility, strength, and long-term safety.
However, the FDA has also recorded complaints and complications related to mesh implants. These include:
Chronic pain
Infection
Mesh migration or shrinkage
Adhesions to nearby organs
Despite this, most patients experience excellent outcomes, especially when procedures are done by skilled surgeons using FDA-approved mesh.
Controversies and Legal Considerations
The medical device industry has faced legal scrutiny over mesh complications, particularly in cases where patients experienced severe side effects. While some mesh products have been voluntarily withdrawn, most complications stem from poor surgical techniques or patient-specific factors.
These issues underscore the need for:
Better patient screening
Enhanced surgeon training
Continued innovation in mesh design
Innovations in Hernia Repair Devices
Thanks to advancements in medical engineering, today’s hernia repair procedures are more sophisticated than ever. Modern mesh designs aim to improve tissue integration, reduce foreign body response, and minimize the risk of complications.
Notable Innovations:
Lightweight and macroporous mesh for better flexibility and lower inflammation
3D mesh shapes for anatomical fit
Resorbable barrier coatings to prevent adhesions in laparoscopic repairs
Robotic-assisted laparoscopic techniques for high precision and less invasiveness
These improvements enhance both functional outcomes and patient satisfaction post-surgery.
Pre-Surgical Considerations and Genetic Testing
Before undergoing any surgical repair, patients are increasingly being encouraged to pursue comprehensive health evaluations. This includes genetic and pre-marital screenings, particularly in high-risk regions.
In places like the UAE, premarital genetic testing has become a standard for detecting inherited disorders that might complicate surgical outcomes or increase the risk of post-operative complications.
➡️ Learn more about how such testing promotes healthier outcomes in this detailed article: UAE Premarital Genetic Testing – Ensure a Healthy Future Together
Risks vs. Benefits: What Patients Should Know
Like all surgeries, inguinal hernia repair with medical devices carries potential risks. However, the benefits typically outweigh the drawbacks, particularly when using advanced mesh and surgical methods.
Common Risks:
Bleeding
Infection
Nerve damage
Mesh-related complications (rare)
Key Benefits:
Long-term durability
Improved quality of life
Less chance of recurrence
Shorter healing period
Patients should discuss all available options with a qualified surgeon and consider a personalized treatment plan.
Post-Operative Care and Recovery
Most patients recover from inguinal hernia surgery within two to six weeks. Medical technology also plays a role in recovery:
Wearable devices help monitor vital signs
Telemedicine follow-ups offer remote checkups.
Digital wound trackers detect infection early.y
With Mostents, retpatientsull activity without complications.
The with proper post-op care and compliance Future of Inguinal Hernia Medical Devices
As technology progresses, the future holds promise for smart implants, nanotechnology, and bioengineered tissues that could completely replace synthetic mesh. Additionally, AI-assisted robotic surgery may soon become the norm in complex hernia repairs, improving precision and outcomes.
Conclusion
Inguinal hernia repair has come a long way from basic suturing techniques to highly advanced medical devices that offer durable, safe, and efficient solutions. Surgical mesh remains a cornerstone of modern hernia surgery, and when used properly, it dramatically enhances the quality of patient outcomes.
By understanding the technologies involved, recognizing potential complications, and choosing the right surgical approach, patients can make informed decisions that lead to successful hernia recovery and a healthier future.